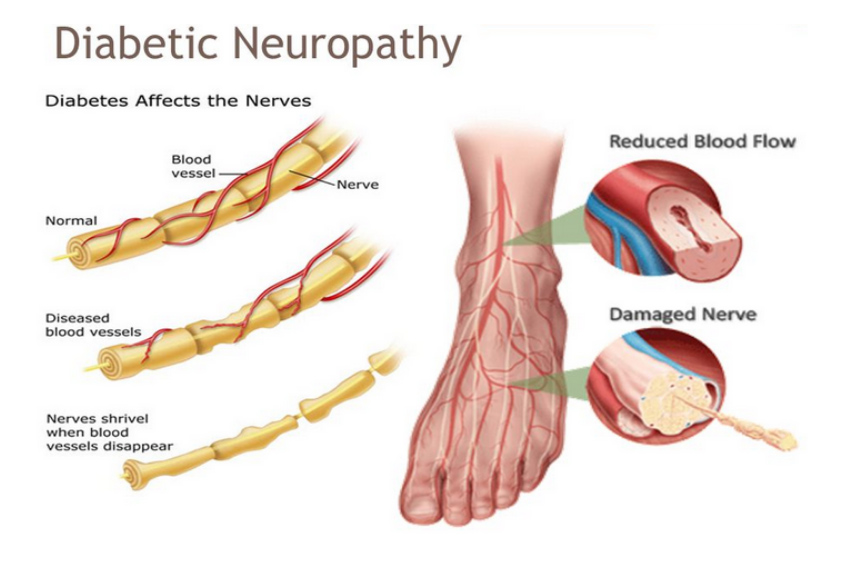
This nerve disorder, linked to diabetes, can cause significant nerve damage. Type 1 and Type 2 diabetes share a typical issue, characterized by excessive blood glucose (sugar) harming the nerves progressively. Diabetic neuropathy tends to progress gradually, affecting multiple nerve systems and causing a variety of signs and issues.
There are several types of diabetic neuropathy, each affecting different types of nerves and causing different symptoms:
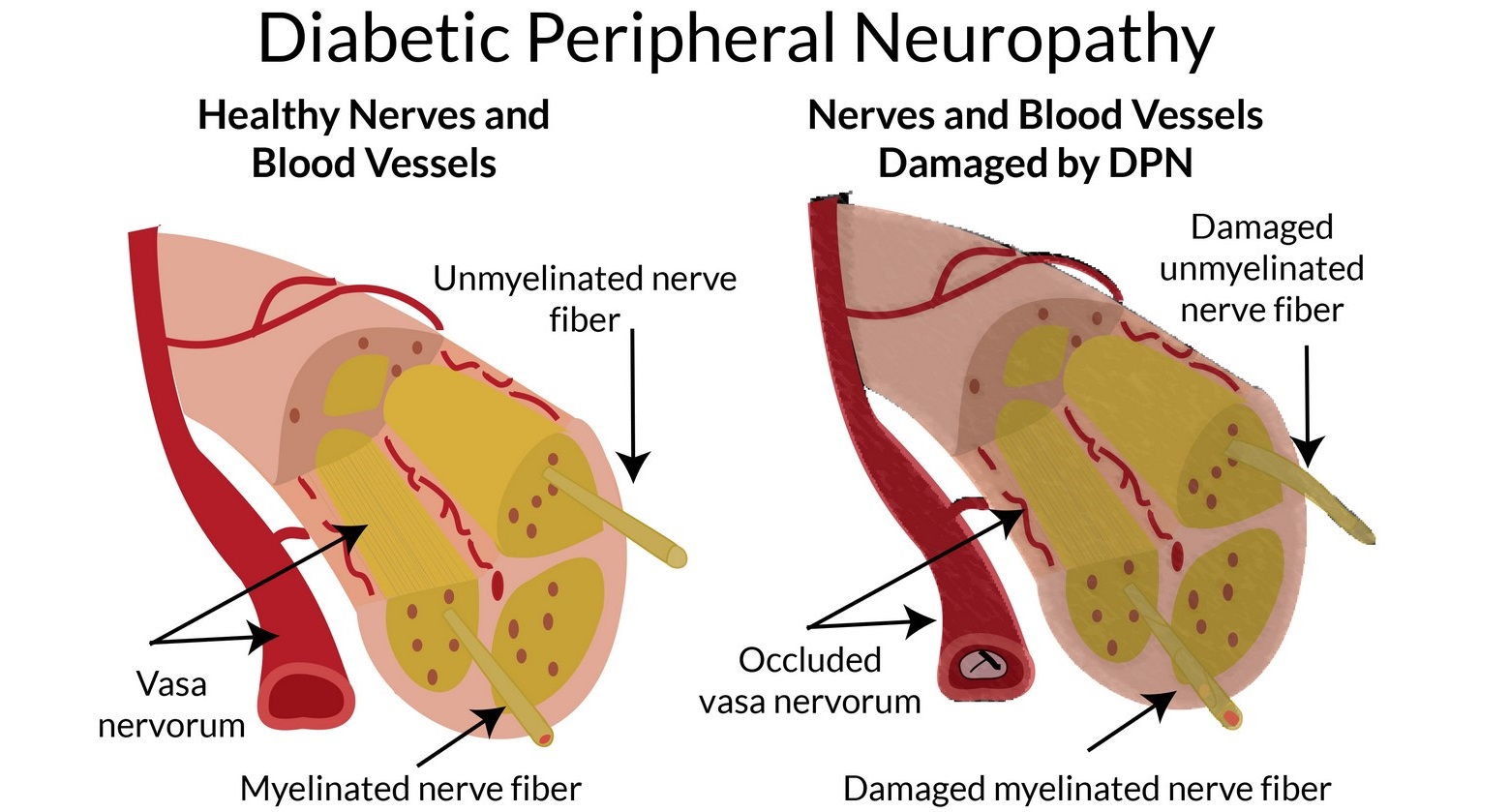
- Peripheral Neuropathy: This is the most common type of diabetic neuropathy and affects the peripheral nerves, which control sensation and movement in the extremities (hands, feet, arms, and legs). Symptoms may include numbness, tingling, burning sensations, pain, and weakness in these areas. Peripheral neuropathy can lead to difficulties with coordination and balance.
- Autonomic Neuropathy: This type affects the autonomic nervous system, which controls involuntary functions like digestion, heart rate, blood pressure, and sweating. Symptoms can include digestive issues, urinary problems, cardiovascular problems (such as heart rate irregularities), and changes in body temperature regulation.
- Proximal Neuropathy: Also known as diabetic amyotrophy, this type of neuropathy affects the muscles of the thighs, hips, buttocks, and legs. It can lead to severe pain, muscle weakness, and difficulty moving these areas.
- Focal Neuropathy: This type involves damage to specific nerves, causing sudden, localized symptoms. For example, carpal tunnel syndrome and cranial nerve palsies (affecting the nerves controlling eye movements) can occur as a result of focal neuropathy.
The risk factors for developing diabetic neuropathy include poorly controlled blood sugar levels, prolonged duration of diabetes, high blood pressure, obesity, and smoking. Monitoring and managing blood sugar levels through lifestyle changes, medication, and insulin therapy are key to preventing or slowing the progression of diabetic neuropathy.
Treatment for diabetic neuropathy involves addressing the underlying cause (poor blood sugar control) and managing the symptoms. Medications can be prescribed to manage pain, and physical therapy might be recommended to improve muscle strength and mobility. Lifestyle changes, such as maintaining a healthy weight, exercising regularly, and controlling blood pressure, can also play a significant role in managing the condition.
It’s important for individuals with diabetes to have regular check-ups with their healthcare providers to monitor and manage their overall health, including the potential development of complications like diabetic neuropathy.