The long-term consequences of high blood sugar on nerve function and blood flow can manifest as diabetic foot problems. If left unchecked, these issues can lead to serious foot conditions, which may result in infections, ulcers, or amputations. Here are some key aspects of diabetic foot problems:
Diabetic Foot Problems
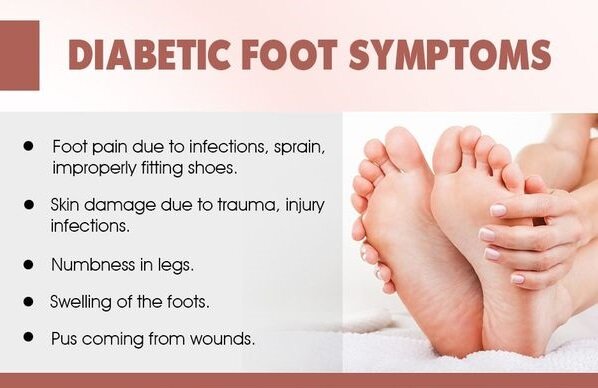
- Neuropathy: Diabetic neuropathy is nerve damage that occurs due to prolonged high blood sugar levels. It often affects the nerves in the feet, leading to loss of sensation or altered sensation. This can cause individuals to not feel pain, heat, or cold properly, which means they might not notice injuries, blisters, or cuts that can become infected if left untreated.
- Vascular Issues: Diabetes can also lead to poor blood circulation, particularly in the extremities like the feet and legs. Reduced blood flow impairs the body’s ability to heal wounds and fight infections. Proper blood flow is essential for delivering nutrients and oxygen to tissues, which aids in wound healing.
- Foot Ulcers: Due to the combination of neuropathy and poor circulation, even minor injuries or pressure points on the feet can develop into ulcers, which are open sores. These ulcers are particularly problematic because they may not heal well and can become infected.
- Infections: Diabetic foot ulcers are susceptible to infections due to the compromised immune response caused by diabetes. Infections can spread rapidly and be difficult to treat, potentially leading to serious complications and the need for amputation.
- Charcot Foot: Charcot foot, also known as Charcot neuroarthropathy, is a condition where bones in the foot weaken and fracture due to neuropathy. The person might continue walking on the foot, worsening the damage. This condition can lead to deformities and significant mobility issues.
- Amputation: If diabetic foot problems are not properly managed and infections are left untreated, amputation of toes, feet, or even parts of the lower leg may become necessary to prevent the spread of infection to the rest of the body.
- Prevention and Management: Proper foot care is crucial for individuals with diabetes. Regular foot inspections, moisturizing, wearing well-fitting shoes, maintaining proper hygiene, managing blood sugar levels, and regular medical check-ups can help prevent or detect foot problems early.
- Treatment: If foot problems occur, a healthcare professional, often a podiatrist or wound care specialist, will provide appropriate treatment. This can include wound care, antibiotics for infections, offloading pressure from ulcers, and addressing circulation issues.
It’s important for individuals with diabetes to work closely with their healthcare team to manage their condition and take proactive steps to prevent diabetic foot problems. Early intervention and proper foot care can significantly reduce the risk of serious complications.
Copyright ©2017 all rights reserved
Designed by Plethora Themes
