Preventing or managing these diabetic eye problems involves several strategies:
- Blood Sugar Control: Maintaining stable blood sugar levels is crucial in preventing or slowing the progression of diabetic eye diseases.
- Regular Eye Exams: People with diabetes should have comprehensive eye exams at least annually, or as recommended by their eye care professional. These exams can detect early signs of diabetic eye diseases and allow for timely intervention.
- Blood Pressure Control: Managing blood pressure levels can help reduce the risk of diabetic retinopathy and other eye complications.
- Lifestyle Choices: A healthy lifestyle that includes a balanced diet, regular exercise, not smoking, and maintaining a healthy weight can contribute to overall eye health.
- Treatment Options: Treatment options vary depending on the specific condition and its severity. Treatments can range from medications and laser therapies to surgical interventions like vitrectomy (removing the vitreous gel from the eye) for advanced cases.
If you have diabetes, it’s important to work closely with your healthcare team and eye care professional to monitor and manage your eye health effectively. Early detection and appropriate management can help preserve your vision and minimize the impact of diabetic eye diseases.
Certainly, I’d be happy to provide more information about diabetic macular edema (DME).
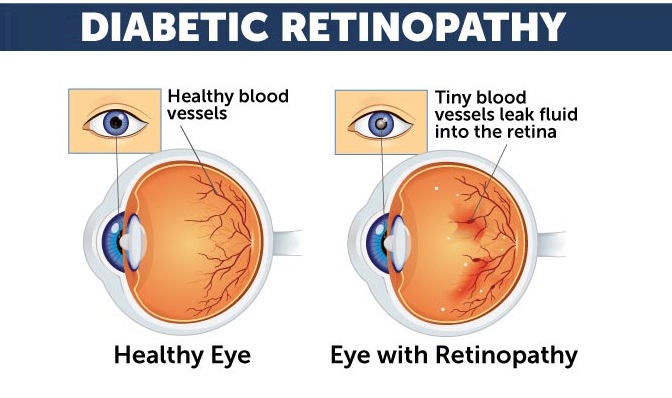
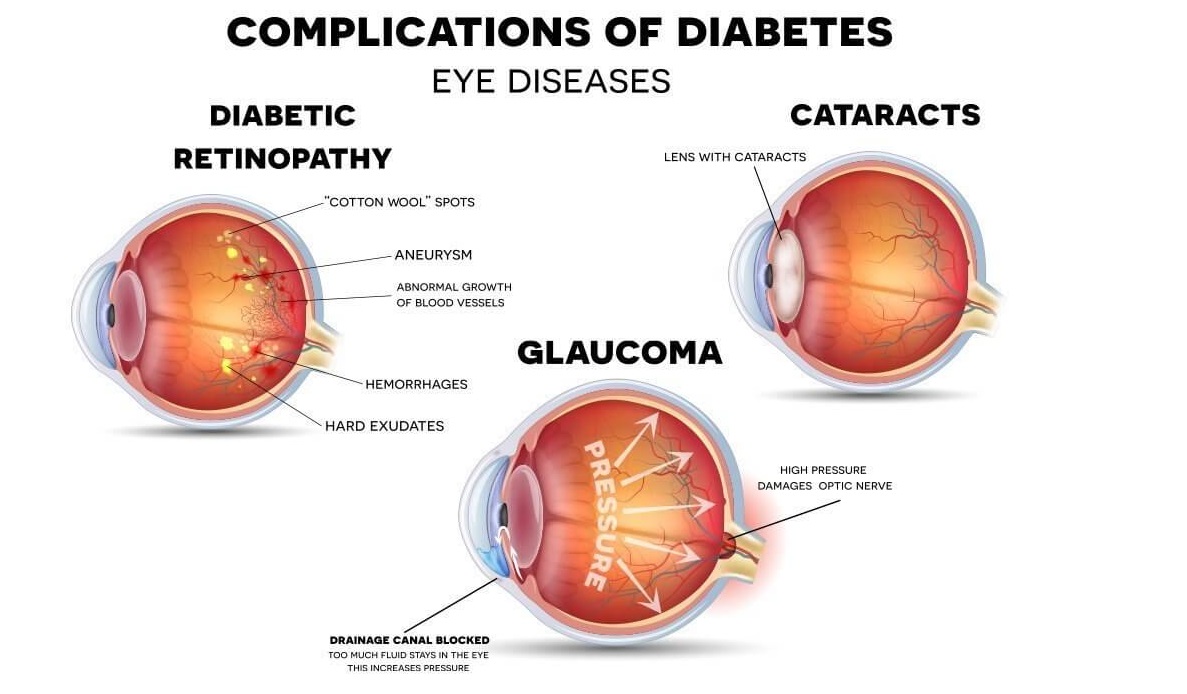
What is Diabetic Macular Edema (DME)? Diabetic macular edema is a complication of diabetic retinopathy, a condition that affects the blood vessels in the retina of the eye. DME specifically involves the swelling (edema) of the macula, which is the central part of the retina responsible for sharp, detailed central vision. The macula is crucial for activities like reading, recognizing faces, and driving.
Causes and Mechanism: High blood sugar levels in diabetes can damage the blood vessels in the retina. In response to this damage, blood vessels can leak fluid and other substances into the surrounding tissues, including the macula. The accumulation of fluid leads to swelling in the macula, causing it to thicken and distort. This distortion disrupts the normal function of the macula, resulting in reduced central vision.
Symptoms: The symptoms of diabetic macular edema can vary, but they often include:
- Blurred or distorted central vision
- Difficulty reading or performing tasks that require fine detail
- Colors appearing washed out or less vibrant
- Visual fluctuations or changes in clarity
It’s important to note that while DME can cause significant vision problems, peripheral (side) vision typically remains unaffected.
Diagnosis: Diagnosis of DME involves a comprehensive eye examination, which may include:
- Visual acuity tests to measure how well you can see at different distances.
- Dilated eye exam to evaluate the retina and macula.
- Optical coherence tomography (OCT), a non-invasive imaging technique that provides detailed cross-sectional images of the retina, including the macula. OCT is particularly useful for assessing the presence and extent of macular edema.
Treatment: The treatment of DME aims to reduce the swelling in the macula and improve or stabilize vision. Treatment options include:
- Anti-VEGF Injections: These are medications that block a protein called VEGF (vascular endothelial growth factor), which contributes to abnormal blood vessel growth and leakage. Anti-VEGF injections are administered into the eye and can help reduce macular edema, improve vision, and prevent further damage.
- Corticosteroid Injections: Corticosteroids are anti-inflammatory medications that can also be injected into the eye to reduce swelling. They work by suppressing the inflammatory response that contributes to the development of macular edema.
- Laser Therapy: Focal or grid laser treatments can be used to seal leaking blood vessels and reduce edema. However, this approach is less commonly used due to advances in anti-VEGF therapies.
Prevention: Managing diabetes effectively and maintaining stable blood sugar levels are crucial in preventing or delaying the onset of DME. Regular eye exams, as recommended by your eye care professional, can help detect early signs of macular edema and allow for timely intervention.
If you have diabetes, it’s important to work closely with your healthcare team and eye care specialist to monitor your eye health and manage any complications, including DME. Early detection and appropriate treatment can significantly improve outcomes and preserve your vision.